A possible cure for type 1 diabetes via stem cell therapy has just entered its third phase of development in June by Vertex Pharmaceuticals, an organization dedicated to creating new medications.
Type 1 diabetes has been known for its lack of a cure, but treatments do exist. Since 1922, people with T1D primarily use artificial insulin as treatment. Treatment changed from that point on, with people using insulin pens, pumps and inhalable insulin. Ten out of 12 people became completely insulin independent, no longer requiring artificial medication, in a single year through the stem-cell therapy experiment by Vertex Pharmaceuticals.
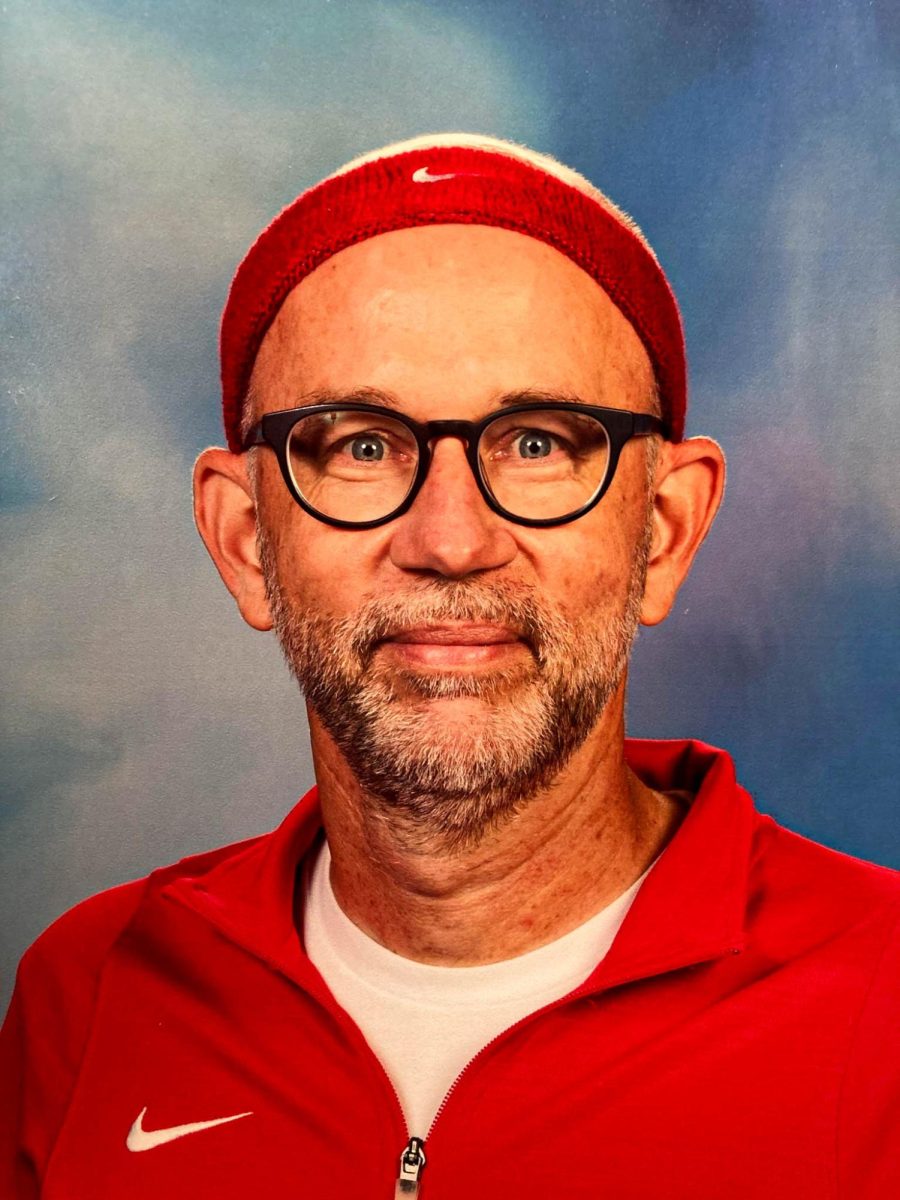
After being diagnosed at the young age of 7 years old, biology teacher and type 1 diabetic Sarah Shado said that living with T1D has just become a part of her daily routine. Shado said that the news of this project was revolutionary.
“My diabetes is a part of me, and it has been for 18 years,” Shado said. “But [regarding the conceptual cure], if there’s a will, there’s a way.”
The stem cell therapy, currently known as Zimislecel, works by injecting genetically modified stem cells into the hepatic portal vein. T1D originates from an issue in the immune system where T cells — a type of white blood cell — view insulin-producing beta cells in the pancreas as dangerous and attack them. The immune system perceives stem cells as harmful foreign objects because it mistakes the stem cells antigens as unrecognizable. In this experiment, participants were put on a regimen of heavy immunosuppressants to prevent the immune system from targeting the stem cells.
“This study seems very risky. I’d worry about some of the potential side effects,” Shado said. “I think it’d be a lot better if the pros and cons were clearer. There’s a lot to think about for such an important topic as this.”
While the idea of a possible cure is hopeful to her, Shado said she has no issues with continuing to live her life as it is, even though her diabetes may be hindering on occasion.
“If they have a cure, that would be great,” Shado said. “Just because of the side effects and timeframe, mostly, I am pretty neutral with the stem cell therapy treatment.”
The most recent results from Phases 1 and 2 of the study include the complete insulin independence of 10 out of the remaining 12 patients within a 365-day period of continuous use of immunosuppressants, and the unrelated deaths of two out of 14 patients. After receiving full doses of Zimslecel, all participants experienced lower HbA1Cs and a lack of severe hypoglycemic events.
Texas Children’s Hospital and Baylor College of Medicine endocrinologist and type 1 diabetic, Daniel DeSalvo said he was concerned in regards to the project’s hazards, especially given his firsthand experiences as a type 1 diabetic and as a doctor and researcher of the field.
“It [is] too dangerous for young, healthy people with T1D right now,” DeSalvo said. “More research and development to improve the safety and effectiveness is needed for this to be a viable long-term solution.”
People with type 1 diabetes have been able to go without insulin. Two people died in the study, with one individual passing from cryptococcal meningitis, and the other from severe dementia. Both cases had to be documented as a precaution and as something to be aware of for the remainder of the study. The documentation of these events is widely available.
“The results are impressive since most participants stopped needing insulin,” DeSalvo said. “My main concern is safety, but my biggest hope is that this could be the first step toward a lasting, practical cure for T1D.”
As a result of the immunosuppression on already weakened immune systems, three of the 12 surviving participants experienced a complication known as neutropenia. This condition is known as a low count of neutrophils, the most common type of white blood cells.
Breakthrough T1D Director of Outreach and Operations and type 1 diabetic Madeline Dicks discusses her ideas in reference to the immunosuppression conflict, and also provides more information surrounding other evolving projects.
“There are a lot of great studies going on regarding insulin independence and immunosuppressants, including some going on right here in Houston.” Dicks said. “There are some studies that have been looking at transplanting islet cells with localized suppression or without immunosuppression.”
Zimslecel was tested specifically on patients with severe hypoglycemic (low blood sugar) events or a limited ability to detect hypoglycemic symptoms. The latter can be dangerous, and hypoglycemia occurs quickly and can cause unconsciousness, seizures or death in a matter of minutes if left unnoticed or untreated. When the 12 patients received full doses of Zimslecel, all patients stopped having severe hypoglycemic events.
“Twenty-five years later, after the introduction of a ‘clear’ long-acting insulin (Lantus), I do all of my T1D management on my phone. I cannot imagine where we will be in another 25 years and it makes me hopeful for a cure,” Dicks said. “The advancements made in technology makes me feel confident that someday a cure is possible.”
Vertex Pharmaceuticals’ initiation of this study into Phase 3 is due to the side effects of the heavy immunosuppressants – and neutropenia. While the study has so far shown great success according to the organization, it is a danger to diabetics, who already have weakened immune systems, by further taking away their protection against illness and other threats. Ten people have already become fully insulin-independent in the century since the creation of artificial insulin.
“Realistically, that ‘pure cure’ might still be 10-plus years away from being safe and widely available,” DeSalvo said. “I hope Vertex [or] other research teams can make a safer version that doesn’t require immune suppression within the next decade.”
Visit https://www.breakthrought1d.org/ to learn more about type 1 diabetes and to keep up with related events in your community.